Side Meetings
SMB112
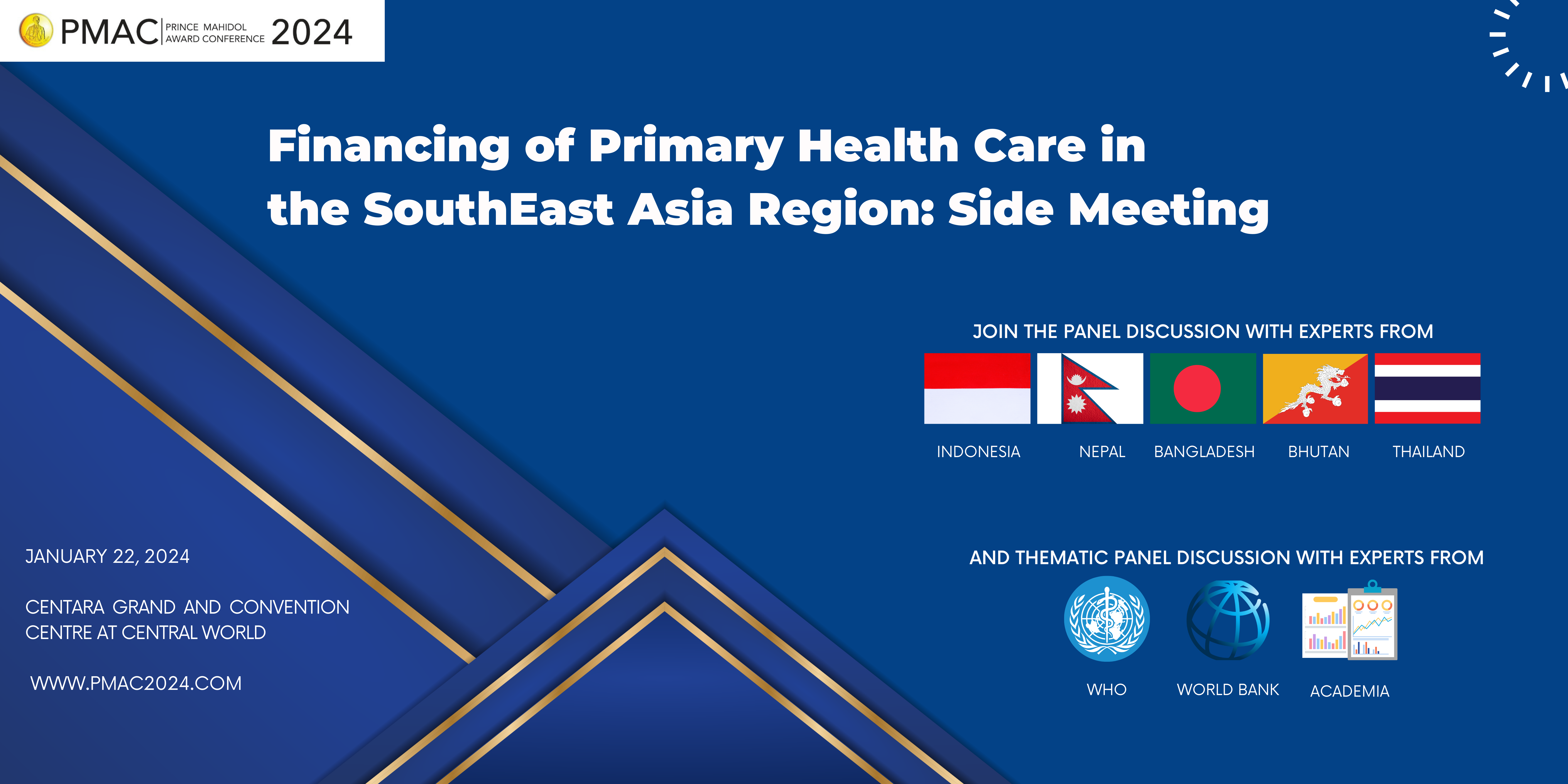
Financing of Primary Health Care in the Southeast Asia Region
22
Jan
- Dr Piya Hanvoravongchai
- Dr Aungsumalee Pholpark
- Dr Hsu Mon
The countries that make up the WHO South-East Asia (SEA) Region are diverse in culture, demography, geography, history and level of socioeconomic development. The Region is also home to more than 2 billion people – over a quarter of the world’s population, including a large share of the world’s poor – with the majority residing in rural areas, but with rapid urbanization taking place across countries. The impact of demographic change is also increasingly felt by countries in the Region, with steady a shift of the population pyramid marked by the aging process. Country health systems in this Region are also at different stages of health sector-related institutional development, which has consequences for the management, financing, capacity and delivery of health services, at the first point of care – PHC. In addition, the role of the public sector in the provision of social services, including health and education, varies considerably across the Region.
Globally and regionally, there has been a strong recognition of the need to prioritize PHC, as seen through the different PHC-focused declarations and strategies – e.g. Declaration of Astana in 2018, Operational Framework for PHC in 2020 and the 2022 approved Regional PHC strategy 2022-2030 (the PHC Strategy), to achieve universal health coverage, health security, and the health-related SDG targets by 2030, through a PHC oriented health system. These strategic and operational guidance have been motivated by the understanding that increased and better public spending on PHC is the most cost-effective way to make progress towards UHC; as 90% of essential health services can be delivered through primary health care and yet, at present, in most countries spending is strongly oriented towards secondary and tertiary care.
The Regional PHC Strategy for the WHO South-East Asia Regional Office has the following objectives, to: a) Support Member States in enabling PHC orientation of their health systems; b) Serve as a resource for stakeholders to engage in PHC transformation; c) Strengthen monitoring of PHC performance and d) Stimulate cross country learning and advocacy. It also has a series of strategic actions and Strategic Action 2 is on health financing to increase and improve PHC financing in the SEA Region.
Public financing of health care is a persisting challenge in the Region. On average, the SEA Region is ranked as the second lowest among all WHO regions in terms of government spending on health which was 3.12% of GDP in 2020. The share of OOP expenditure for the Region remains the highest among all WHO regions, at 38.5% of health expenditure, in 2020. In some countries, the share of out-of-pocket expenditure is very high, and in others it has even been increasing, while some others have succeeded in keeping out-of-pocket expenditure at or below 20%. Public financing is the predominant source of financing in some countries, as seen in Bhutan, Maldives and Thailand. Social health insurance is only a small source of health financing in most countries except for Indonesia, where social health insurance is growing in significance.
Of the seven countries with data, the expenditure on primary health care (PHC) as a percentage of GDP constituted a very small fraction of GDP. This highlights the urgent need for additional financial allocations for PHC, and improved monitoring of PHC investments in order to ensure sufficient financing for high-quality primary care systems among countries in the Region.
While there is some information, on how PHC systems are financed in the different countries of the region, most of this is not systematized and gathered around a robust conceptual framework that allows us to analyse the systems, draw adequate conclusions and provide pertinent recommendations. On the one hand, countries in the region are quite heterogenous and to provide more tailored and actionable recommendations to the specific context of countries, a selected group is being chosen for a more focused analysis which will entail more extensive key informant interviews covering a broader set of stakeholders and perspectives for each of the countries in the group. Hence, our approach is to prioritise at this stage, greater depth of analysis as opposed to breath of country coverage across the region. The selected group of countries are those that have a considerable presence of private providers, so mixed health systems, and some elements of health insurance, be it social health insurance (as in the case of Indonesia, the Maldives and Nepal) or government sponsored insurance schemes (such as Bangladesh). India also has government sponsored health financing, but the diversity of its health systems with state-led mechanisms may be too complex for the time available for this study. Therefore, the group of selected countries are: Bangladesh, Indonesia, Maldives, and Nepal. Thailand also has a considerable private sector presence in its health service delivery system and has different health insurance schemes; but it also has a vast body of evidence documenting its financing aspect and is the country in the region that has made greatest progress towards UHC. While it will not be subject to in-depth analysis, particularly drawing on several key informant interviews, published literature on Thailand will be drawn on for comparative purposes and for illuminating the findings on the selected four countries for this work.
Objective 1: To present the results of a review of existing literature on financing of PHC of 11 countries in the WHO South East Asia Region: Bangladesh, Bhutan, Democratic People’s Republic of Korea, India, Indonesia, Maldives, Myanmar, Nepal, Sri Lanka, Thailand, and Timor-Leste.
Objective 2: To explore bottlenecks and good practices of financing of PHC of four selected countries (Bangladesh, Indonesia, Maldives and Nepal).
Objective 3: To gain insights and lessons through a technical expert panel discussion on: a) sources and level of financing for PHC; b) purchasing mechanisms for PHC; and c) political economy dynamics of PHC financing reforms.
Objetive 4: To reflect on recent policy directions for countries moving towards primary health care oriented financing reforms based on the global evidence.

